Many women don’t realize they have a fallopian tube blockage until they run into trouble getting pregnant. But fallopian tube problems actually account for 10 to 15% of female infertility.
Blocked or scarred tubes can make it difficult for sperm to reach and fertilize an egg. Fortunately, there are treatment options that can help you conceive.
Here’s what you should know about this condition, also known as a hydrosalpinx, including where it comes from, how it’s treated, and what you can do to increase your chances of getting pregnant.
What causes blocked fallopian tubes?
A fallopian tube can get blocked when adhesions form within a tube or between the end of a tube and an ovary. These blockages can result from a few different health issues,[1] including:
- Pelvic inflammatory disease (PID). PID is a bacterial infection affecting the uterus, fallopian tubes or ovaries. The infection can cause inflammation and potentially the formation of scars and blockages in the fallopian tubes, especially when left untreated.
- Sexually transmitted diseases. Bacterial STDs like chlamydia and gonorrhea can cause PID, triggering scarring and blockages.
- Endometriosis. With endometriosis, uterine tissue grows in places where it shouldn’t — like the fallopian tubes. These growths can cause blockages or lead to scarring.
- Abdominal or pelvic surgery. Any surgery in the lower belly or pelvic area — including surgery to remove uterine fibroids or ovarian cysts — has the potential to cause scar tissue that leads to a tube blockage. A ruptured appendix caused by appendicitis could lead to scarring as well.
What are the signs of blocked fallopian tubes?
A blocked fallopian tube, or hydrosalpinx, often goes completely unnoticed and doesn’t usually have any symptoms. For example, you can still have completely normal periods with a blockage, and the blockages are typically not painful.
Read This Next
Fallopian tube blockages can cause female infertility, however — so for many women, trouble getting pregnant is usually one of the first signs. Women with a blockage might also be more likely to experience an ectopic pregnancy.
In some cases, a hydrosalpinx may cause discomfort. Some women experience regular pain in their belly or pelvic area that tends to get worse during their periods. Occasionally, unusual vaginal discharge can be a symptom of blocked fallopian tubes.
How to find out if your fallopian tubes are blocked
Most practitioners diagnose fallopian tube blockages with a procedure called a hysterosalpingogram or HSG test.[2]
This short test, which can be done in your provider’s office, involves injecting a liquid dye into the uterus and taking X-rays to see how the liquid moves through the fallopian tubes. If the liquid backs up or causes the tubes to stretch or swell, there’s a blockage.
In some cases, your provider might opt to look at a blockage via laparoscopic surgery. You may also sometimes see larger blockages on an ultrasound.
Treatments for blocked fallopian tubes
If a hydrosalpinx has affected your fertility, addressing the blockage can usually increase the chances of becoming pregnant. There are a few different ways to do that based on where your blockage is located and if it can easily be removed.
Surgery
Depending on the cause and severity of the blockage, your provider may remove the scar tissue that’s causing the block, make a new opening outside of the blocked tube that’s near the ovary, or open the tube from the inside by breaking up the blockage.
Some blockages can be removed laparoscopically, while others require traditional surgery with a larger incision.
In vitro fertilization
Surgery may not effectively repair severely damaged fallopian tubes. In that case, your provider may recommend bypassing the blockage altogether and trying to get pregnant via in vitro fertilization (IVF).
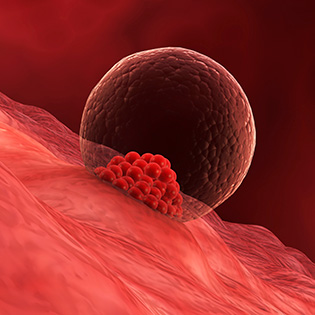
During in vitro fertilization, mature eggs are collected from your body and fertilized by sperm in a lab. Then one or more of those fertilized eggs (embryo or embryos) is transferred into the uterus with the hope it will implant and result in a pregnancy — and a baby nine months later.
Hysterosalpingogram (HSG)
HSGs typically diagnose blocked fallopian tubes, not treat them.
But some studies have shown that some women with mild to moderate blockages who undergo HSG tests may conceive within three to six months after the procedures.
Experts don’t fully understand why, but one potential explanation is that the dye used to detect the blockage helps flush out the fallopian tubes.
Complications from blocked fallopian tubes
Scarred, inflamed or partially blocked fallopian tubes increase the risk of an ectopic pregnancy. In fact, up to 50% of ectopic pregnancies occur in women who have tube abnormalities.
An ectopic pregnancy happens when a fertilized egg implants outside of the uterus — usually in one of the fallopian tubes. Ectopic pregnancies are never viable, and when left untreated they can cause serious and even life-threatening complications like internal bleeding.
If you’ve recently had tubal surgery, you should call your provider right away if you notice possible symptoms of an ectopic pregnancy — including abnormal bleeding or brown spotting after a positive pregnancy test, sharp or crampy abdominal pain that gets worse when you move, or lower back pain.
Other possible risks associated with any type of surgery include infection or bleeding, an allergic reaction to the anesthesia (or dye, if you’re having an HSG test), or the formation of new scar tissue.
Prevention
You can’t always prevent blocked fallopian tubes, especially if the blockage forms as the result of endometriosis or another abdominal or pelvic surgery. But you can take steps to possibly reduce your risk for other blockage culprits like pelvic inflammatory disease, chlamydia and gonorrhea.
- Avoid douching. It can disrupt the normal bacteria in your vagina, putting you at higher risk for infection.
- Practice safe sex. Use condoms when you have sex, and ask partners about their sexual history.
- Get tested for STDs if you need to. Women under 25 should get tested for chlamydia and gonorrhea every year; women over 25 with new or multiple sex partners should also receive tests annually. If you’re at risk for gonorrhea or chlamydia, you should also be tested during early pregnancy. Your doctor can help determine your individual risk and advise when you should be tested.









































 Trending On What to Expect
Trending On What to Expect





