Bleeding after delivery is normal. In fact, women usually lose about half a quart of blood during a vaginal birth and one quart of blood after a C-section.
But when you lose excessive amounts of blood after childbirth — called a postpartum hemorrhage (PPH) — you can experience dangerous complications like a drop in blood pressure and even shock (when your body’s organs don’t get enough blood).
What is postpartum hemorrhage?
Postpartum hemorrhage is excessive, uncontrolled blood loss that usually occurs within a day after giving birth, but can sometimes take place up to 12 weeks after delivery. The bleeding can be from the site where the placenta was attached to the uterus, or can stem from unrepaired vaginal or cervical tears.[1]
An infection can also trigger a postpartum hemorrhage in the days or weeks following delivery.
How common is postpartum hemorrhage?
Postpartum hemorrhage is a relatively rare but serious condition, occurring in up to 5% of deliveries. Typically women lose about half a quart of blood during vaginal birth and a quart of blood during a C-section procedure. With postpartum hemorrhage, the bleeding is severe and often causes a change in heart rate or blood pressure.
The condition can be more likely to happen if you’ve had bleeding during your pregnancy. The good news is when caught early it can be successfully treated.
What are the two types of postpartum hemorrhage?
There are two kinds of postpartum hemorrhage. The first, called primary postpartum hemorrhage, is excessive bleeding within the first 24 hours after delivery. It frequently occurs right after baby is born or your placenta is delivered.
The most common cause of this sort of hemorrhage, which accounts for about 80% of cases, is when your uterus doesn’t contract as it should during or after giving birth, also called uterine atony. Other reasons for a primary postpartum hemorrhage include unrepaired or cervical lacerations, retained tissue, placenta abnormalities, and bleeding disorders.
Read This Next
The other kind is called secondary or late postpartum hemorrhage, which occurs 24 hours to 12 weeks postpartum. This is a rare type of hemorrhage and makes up only about 2.5% of all cases. It happens when a part of the placenta stays attached to the uterine wall and isn’t fully expelled by your uterus.
Normal discharge (lochia) vs. postpartum hemorrhage: What’s the difference?
Normal lochia (i.e., postpartum bleeding/discharge) tends to be darker in color — somewhat like your menstrual period, only heavier. The blood from a postpartum hemorrhage, on the other hand, can be bright red in color and excessively heavy, causing you to soak through more than one a sanitary pad an hour, and is accompanied by symptoms of low blood pressure, like dizziness, breathlessness, or a racing heart.
Normal postpartum bleeding signs include:
- Dark red blood that can last for up to 10 days after giving birth
- Light bleeding and spotting that can last for up to four to six weeks after delivery
Some of the symptoms of a postpartum hemorrhage include:
- Soaking through more than one sanitary napkin an hour
- Bright red bleeding for more than a few days
- Passing very large blood clots (think: the size of a lemon or larger)
- Faintness, breathlessness, dizziness, or a racing heart
- Nausea or vomiting
- Swelling and pain around the vagina or perineum (the area in between the vagina and rectum)
If you notice abnormally heavy bleeding during the first week or two postpartum, or are experiencing the symptoms of a postpartum hemorrhage, call your practitioner immediately. If you can’t get in touch with your doctor, call 911.
Who is most at risk for postpartum hemorrhage?
Some pregnancy complications can increase your risk for postpartum hemorrhage, including:
- Having a uterus that doesn’t contract well after birth. Uterine contractions help stop the bleeding from the area where the placenta breaks away from the uterus.
- Having a uterus that becomes overdistended. This can be due to carrying twins, carrying a large baby, or having excessive amniotic fluid (hydramnios).
- Intraamniotic infection (or chorioamnionitis), an infection of the membranes that can occur during labor.
- Uterine inversion, a rare childbirth complication that occurs when part of the uterine wall collapses and turns inside out.
- Uterine rupture, when an area of the uterine wall tears during labor.
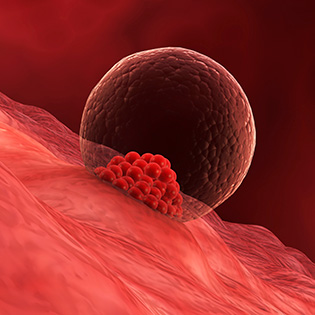
- Placenta previa, a pregnancy complication in which the placenta implants low in the uterus, or placenta accreta, a condition where the placenta grows into the wall of the uterus.
- Placenta abruption, when the placenta separates from the uterine wall before delivery.[2]
- Having large uterine fibroids.
- Taking drugs or herbs that interfere with blood clotting, such as aspirin, ibuprofen, ginkgo biloba, or large doses of vitamin E.
- Having a bleeding disorder such as Von Willebrand’s (in which your blood doesn’t clot as it should) or other health conditions.
About 40% of postpartum hemorrhages occur in women with no risk factors.
How is postpartum hemorrhage diagnosed?
You or your doctor or nurses may notice the symptoms of postpartum hemorrhage while you're still in the hospital. Your doctor may also do a pelvic exam to check your uterus as well as measure the volume of blood or weigh the number of blood-soaked pads and sponges used during delivery to determine exactly how much blood you have lost.
Your doctor will also access your health history and monitor your blood pressure and heart rate to check for any problems.
What are potential complications of postpartum hemorrhage?
Postpartum hemorrhage is responsible for approximately 10% of all pregnancy-related deaths. While most women recover well, an untreated postpartum hemorrhage can lead to a severe drop in blood pressure that can cut off blood flow to vital organs and lead to shock and even death.
The loss of large amounts of blood can make you feel faint, breathless or dizzy, or cause your heart to speed up. If you experience these symptoms, be sure to alert your health team or call 911 so that you can get immediate treatment.
How is postpartum hemorrhage treated?
The treatment for postpartum hemorrhage depends on the cause. For the most common cause of hemorrhage, uterine atony, your doctor may massage your uterus to encourage it to contract and suggest that you begin breastfeeding as soon as possible, if you are planning on doing so, which will also help your uterus to contract.
Additionally, there are medications that your provider can use to help stimulate a uterine contraction, as well as devices that can be placed within your uterine cavity to stop bleeding with pressure.
After the placenta is delivered, your practitioner will examine it to make certain that it’s complete — that no part of it is remaining in your uterus. An ultrasound can help assess the situation. When part of the placenta is still attached to the uterus, it is a risk factor for postpartum hemorrhage.
If the bleeding is severe, you may need intravenous fluids (IV) or possibly even a blood transfusion.








































 Trending On What to Expect
Trending On What to Expect





