A break from monthly bleeding is one of the perks of pregnancy, so it’s definitely unsettling if you spy blood once you’ve conceived. But spotting or bleeding isn't always a sign of something wrong. In fact, up to 25 percent of women experience it in the first trimester, according to the American Academy of Family Physicians, and more than half go on to have healthy pregnancies and babies.[1]
So if you notice blood down there, you can take a deep breath and read on for a probable (and probably reassuring) explanation. Here’s more about the difference between spotting and bleeding, what causes it during pregnancy, and how it’s treated when you’re expecting.
How can you tell the difference between spotting and bleeding?
The difference usually comes down to the shade of the blood and the amount of it. In terms of color, spotting is often brownish or pink, similar to what you’d expect at the end of your period. As for amount, you’re probably spotting if the blood is so light that you reach for a panty liner rather than a maxi pad.
On the other hand, bright red blood is considered bleeding, especially if it’s flowing and heavy. If you’re experiencing bleeding during pregnancy, you’ll skip over that box of liners in favor of a sanitary pad to protect your clothes.
What causes spotting during pregnancy?
Light spotting is common and usually benign, and can begin around week 3 or 4 of pregnancy. But spotting can happen anytime during these nine months, from the early days of fertilization up to your due date. Here are some of the common causes of spotting during pregnancy:[2]
Read This Next
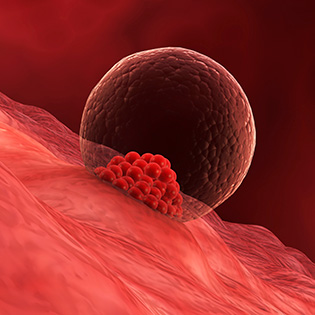
- Implantation bleeding. The implantation of the embryo into your uterine wall usually occurs before or around the time you expected your period, or about six to 12 days after conception. Implantation bleeding is lighter than a period, lasts from a few hours to a few days, looks pinkish or brownish and isn’t a sign of something wrong.
- Sex. Any kind of minor impact down there — like getting busy between the sheets — may irritate your already tender cervix, which has become engorged with blood vessels, and cause light bleeding. This spotting is pretty common, but do tell your practitioner if you’d like extra reassurance.
- Internal pelvic exam or Pap smear. The same type of spotting you might see after sex is also possible when your doctor performs an internal exam or Pap smear.
- Infection of the vagina or cervix. An infection can irritate or inflame the cervix, causing it to bleed a little (though the spotting should disappear once you're treated).
- Loss of mucus plug. This barrier seals your cervix, but later in pregnancy it falls out, indicating the start of labor. It’s usually clear and sticky, but it may also be brown or yellow.
- Subchorionic bleed. Blood accumulates within the folds of the chorion — the outer fetal membrane, next to the placenta — or between the uterus and the placenta itself, causing light to heavy spotting. In most cases, it resolves on its own and isn’t a problem in pregnancy.
Taking note of any spotting during early pregnancy in the What to Expect app can help you determine whether the cause is implantation bleeding or something else.
What causes bleeding during pregnancy?
Period-like bleeding early in pregnancy, or at almost any time, can signal that something is up. Because heavier bleeding may go hand in hand with any number of pregnancy complications, pinpointing the exact reason is best left to your practitioner. Here are a few possible causes:
- Ectopic pregnancy. This nonviable pregnancy occurs when a fertilized egg implants outside of the uterus, usually in the fallopian tubes. Oftentimes, ectopic pregnancies are found about four to six weeks into the pregnancy, but if you’re noticing symptoms — like heavier vaginal bleeding and severe sharp abdominal pain that’s sometimes accompanied by rectal pressure, shoulder pain, lightheadedness, or fainting or shock — seek immediate medical attention.
- Molar pregnancy. Typically discovered within weeks of conception, a molar pregnancy is when a placenta becomes a mass of cysts accompanied by a malformed or nonexistent embryo. Signs of this rare condition include dark brown to bright red vaginal bleeding with severe nausea, vomiting and cramping.
- Miscarriage. This early loss, before 20 weeks, happens in about 10 percent of pregnancies and is most often related to a chromosomal or other genetic defect of the embryo, though it may also be due to hormonal or other factors. Heavy vaginal bleeding (possibly with clots and/or tissue) may occur with severe cramping, lower belly or back pain and a sudden, pronounced decrease in early pregnancy symptoms, like breast tenderness and morning sickness, that differs from the gradual diminishing as the first trimester ends.
- Placenta previa. While usually discovered on a second trimester ultrasound or possibly in the third, this relatively rare complication happens when the placenta implants on the lower part of the uterus and covers part or all of the cervix. (In most women, the placenta moves up and away before birth.) When placenta previa is accompanied by bright red bleeding, your practitioner will likely put you on pelvic rest (meaning no sex) and advise you to relax and avoid strenuous activity or exercise.
- Placenta accreta. If placenta previa is suspected or diagnosed, you may also be monitored for placenta accreta, which occurs when the placenta attaches too deeply in the uterine wall.
- Placental abruption. This condition, which almost always occurs in the second half of pregnancy and usually in the third trimester, is the early separation of the placenta from the uterine wall. In addition to light to heavy bleeding with or without clots, you may also notice abdominal aching or cramping, uterine tenderness and pain in the back or abdomen. If the separation is slight, there's usually little danger to you or your baby and you'll probably be monitored closely and told to take it easy. But if it's more severe, you may need to be hospitalized — which is why it's so important to see your doctor regularly.
- Preterm labor. If you go into labor after week 20 and before week 37 of pregnancy, it’s considered preterm. Along with bleeding, it can be accompanied by other labor signs including back pressure, unusual pelvic pressure and regular contractions that intensify and become more frequent even when you change positions. If you suspect labor is starting early, contact your practitioner immediately.
- Uterine rupture. It’s possible for the uterus to tear during labor, causing bleeding, though this is very rare. Women who’ve had a prior cesarean birth or other uterine surgery that’s left a scar are most at risk.
When should you worry about spotting or bleeding during pregnancy?
Concern about bleeding during pregnancy is completely normal. Light spotting is as variable as it is common, and while it’s usually nothing to worry about, it’s a good idea to call your doctor and let him or her know. Some women spot on and off for their entire pregnancies, while others spot for just a day or two or a few weeks. Happily, most women continue to have healthy pregnancies and healthy babies.
Heavier bleeding also warrants a call to your practitioner, especially if it's accompanied by cramps or pain in your lower abdomen. But it's not inevitably a sign that you're miscarrying. Some women bleed, even heavily, for unknown reasons and still deliver healthy babies.
What is the treatment for spotting and bleeding during pregnancy?
In addition to an exam and various tests at the doctor’s office, rest and relaxation are often the best treatments for a case of spotting or bleeding during pregnancy. That might include some time away from work, getting help with little ones and chores at home, and skipping sex for a while.
More serious cases may require a hospital visit or surgery, depending on the diagnosis. If your blood type is Rh negative, you’ll get an injection of RhoGAM if Rh incompatibility is diagnosed during your pregnancy.
When should I go to the doctor for spotting or bleeding during pregnancy?
You shouldn’t hesitate to talk to your physician about spotting or bleeding, no matter how much (or little) there is, even if it’s during the first trimester. Depending on whether or not you’re experiencing any other symptoms, your doctor may want to see you right away or advise you to call back if the bleeding doesn’t go away.
If your doctor does want you to come in for an appointment, you may receive a blood test to check hCG levels or an ultrasound to check and see that your pregnancy is progressing.
Bleeding during the second trimester, even if it’s not much, should always be discussed with your health care provider the day it happens. And if you spy blood during the third trimester, get in touch with your doctor right away.
No pregnant woman wants to see vaginal blood of any amount or shade when she’s expecting, but much of the time, spotting or light bleeding isn’t a serious problem. Keep track of your symptoms and speak with your doctor at any point for reassurance and guidance.








































 Trending On What to Expect
Trending On What to Expect





