There's a lot of good news for pregnant women with type 2 diabetes, a condition in which the body doesn't respond as it should to insulin.
In fact, with the right medical help and diligent self-care, you have about the same excellent chances of having a successful pregnancy and a healthy baby as any other expectant mom.
The key to managing type 2 diabetes during pregnancy? Achieving normal blood glucose (sugar) levels six months before conception and maintaining those levels throughout the nine months following it.
So if your diabetes has been under control, it's more important than ever to continue your routine now that there are two of you on board. Here's what to think about if you're heading into pregnancy with type 2 diabetes.
How does diabetes during pregnancy affect babies?
If you have type 2 diabetes, you have higher levels of glucose circulating in your blood, and health issues can arise if your blood sugar levels aren't well monitored and managed.
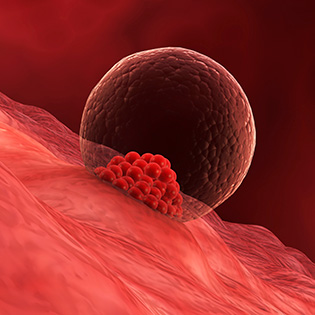
That's because extra sugar can be transferred to baby while you're expecting — and a fetus that's served too much glucose reacts by producing an increased supply of insulin (which can result in a too-large baby and other complications).
Finding your pregnancy and diabetes care team
Be prepared: You'll have a lot more prenatal visits than other expectant moms and will probably be given more doctors' orders to follow (all for a good cause).
So it's a smart idea to get your medical team in place as soon as you think you might want to get pregnant. Check to make sure that your OB/GYN or midwife has plenty of experience caring for diabetic moms-to-be. He or she should work together with the doctor who has been in charge of your diabetes.
The following people can help you to manage your condition and stay healthy (though you may not need or choose to see all of these practitioners)
Read This Next
- An endocrinologist. You may already see this doctor, who specializes in treating people with diabetes (or may be working with an internal medicine doctor). If you're not, ask your primary care doctor if you should consider finding one who can help you monitor your blood glucose levels throughout pregnancy.
- A high-risk OB/GYN. If you have type 2 (or type 1) diabetes, try to find an OB/GYN who specializes in treating women with diabetes; he or she can discuss your risk factors and ways to avoid complications.
- A nutritionist. You'll want an attainable diet geared to your personal requirements; a nutritionist (along with the rest of your team) can help you come up with the right meal plan. Ideally, you'll start your diet pre-pregnancy — and you'll want to follow up after conception to make adjustments. If you don't already work with a nutritionist, ask your doctor for a recommendation or find a professional through the Academy of Nutrition and Dietetics.
- A certified diabetes educator (CDE). A CDE is a health professional who has expertise in prediabetes, diabetes prevention and management. He or she can offer individualized plans to help you better understand and manage your condition; visit the National Certification Board for Diabetes Educators to find a CDE near you.
- A specialist pediatrician or neonatologist. It's not a bad idea in your second trimester to start looking for a children's doctor who specializes in treating the children of women with diabetes.
Controlling diabetes during pregnancy
One of the best ways to have a healthy pregnancy is to get your body in the best possible shape for making a baby before — and after — conceiving.[1]
That means doing the following:
1. Fine-tuning your diet during pregnancy
Diabetic pregnant moms can expect to follow a meal plan similar to the typical pregnancy diet, including a balanced mix of complex carbohydrates and protein. Your diet should also be low in cholesterol and fat and contain few sugary sweets.
Plan your diet with personal preferences in mind but also under the guidance of your physician, a nutritionist and/or a nurse-practitioner with expertise in diabetes.
Here are a few tips for pregnant women with diabetes:
- Keep a close eye on carbs. If you are on oral diabetes medications, you may need to pay slightly closer attention to your sugar levels than those who are taking rapid-acting insulin. The extent of your carbohydrate restriction will depend on the way your body reacts to particular foods. Most women with diabetes do best getting their carbohydrates from vegetables, whole grains and legume sources rather than from fruit. Ask your doctor about the right number of carbs to keep your blood glucose levels in check. It may not be as strict as it used to be for those on fast-acting insulin, which can be adjusted if you go over your limit.
- Snack smart. Snacks will also be important (even more important than they are for the average mom-to-be), and ideally, they should include both a complex carbohydrate (such as whole grain bread) and a protein (like beans, cheese or chicken).
- Eat frequently. Skipping meals or snacks can dangerously lower blood sugar, so try to eat on schedule, even if morning sickness or indigestion are putting a damper on your appetite. Eating six mini-meals a day that are regularly spaced, carefully planned and supplemented as needed by healthy snacks is your smartest strategy.
2. Gaining the right amount of weight
It's best to try to reach your ideal weight before you plan to conceive. But if you start your pregnancy overweight or obese, it will be extra important to set a weight gain goal with your practitioner and to stick to it (think: slow and steady). Gaining too much weight can put you at risk of other pregnancy complications, so be sure to keep an eye on the scale.
Your baby's growth will also be monitored using ultrasound. That's because babies of diabetics sometimes grow very large, even if mom's weight is on target.
Heavier babies make delivery more difficult (there's a higher chance of childbirth complications and/or cesarean delivery when baby is very large). Research shows babies who are bigger than average at birth are also more likely to be overweight as adults, which puts them at a higher risk of diabetes, heart disease and other illnesses.
3. Fitting in fitness
A moderate exercise program will give you more energy, help regulate your blood sugar, keep your weight gain on track and get you in good shape for delivery. But it must be planned with your doctors in conjunction with your diet and medication regimen.
If you have no other complications and are physically fit, moderate exercise — brisk walking (but not jogging unless you were a jogger before you got pregnant), swimming and riding a stationary bike — will likely be on the workout menu.
Chances are that only very light exercise (leisurely walking, for instance) will get the green light if you were out of shape before getting pregnant or if there are any signs of problems with your diabetes, your pregnancy or your baby's growth.
The precautions you take during exercise probably won't differ much from those of any other pregnant woman: Have a snack before your workout, don't exert yourself to the point of exhaustion and never exercise in a very warm environment (80 degrees Fahrenheit or higher).
If you're on insulin, you'll probably be advised to avoid injecting it into the parts of the body you're using in your workout (your legs, for example) and told not to reduce your insulin intake before you exercise.
4. Getting enough rest
Getting enough sleep and rest is important, especially in the third trimester. Avoid overdoing it, and if you can, try to take some time off to put your feet up or power nap during the middle of the day.
5. Regulating medications
If diet and exercise alone don't control your blood sugar, you'll likely be put on insulin (if you aren't already).[2] If you end up needing it for the first time during pregnancy, your blood sugar can be stabilized under close medical supervision.
If you were taking oral medication before you conceived, you might be switched to injected insulin or an under-the-skin insulin pump during pregnancy.
Since levels of the pregnancy hormones that work against insulin increase as pregnancy progresses, your dose may have to be adjusted upward periodically.
How much you need may also have to be recalculated as you and your baby gain weight, if you get sick or are under extreme emotional strain, or if you overdo your carbs.
Studies show that some oral medications may be effective alternatives to insulin therapy during pregnancy for some mild cases, but work with your doctor to make sure your regimen is best for you and your specific situation.
In addition to being sure your diabetes medicine is on target, you'll need to be extremely careful about any other medications you take. Many over-the-counter drugs can affect your insulin levels — and some medications may not be safe in pregnancy — so don't take any until you check with both the physician overseeing your diabetes and the one taking care of your pregnancy.
6. Regularly checking your blood sugar levels
You may have to test your blood sugar at least four to 10 times a day, possibly before and after meals, to ensure it's staying within safe levels. Special sensors and pumps, a simple finger-prick method or tracking apps can all be helpful in monitoring and regulating your sugar intake.
That said, make sure to always check with your practitioner to understand your blood glucose numbers and keep these general guidelines in mind:
- Before a meal your fasting blood sugar number should be in the 60 to 99 mg/dl range.
- One to two hours after eating the numbers should be 100 to 129 mg/dl.
You may be told to write down the results along with what you've been eating throughout the day. One of the best ways to continuously stay on top of your glucose levels is by having a tiny sensor placed under the skin of your tummy. The device collects readings automatically every five minutes or so and sends the information to a wireless wearable monitor or app. If your sugar drops to a dangerously low level, an alarm will sound, activating an insulin pump.
If you were insulin-dependent before pregnancy, you may be more subject to low blood sugar episodes (hypoglycemia) than when you weren't pregnant, especially in the first trimester — so careful monitoring is a must.
And don't leave home without packing the right snacks. If you notice your numbers continue to be too low or too high and you continue to have difficulty regulating your blood sugar levels, call on your doctor for guidance. It's why he or she is there.
7. Careful monitoring by your doctor
To make sure all is going well, you'll be watched more carefully during your nine months than other moms-to-be. Translation: You'll need to have checkups and more routine tests, which aside from any inconvenience is a good thing overall.
Along with regular blood screenings, here are some of the exams you can expect:
- Urine tests. Your practitioner may check your urine regularly for ketones. These are acidic substances that can result when your body breaks down fat. If the levels are too high they can be dangerous for baby, so your doctor will want to keep an eye on it. Your urine will also be tested regularly for protein (sometimes over 24 hours) to make sure your kidney function is up to par.
- Eye exams. You'll probably have an eye exam within the year to check the condition of your retinas. Retinal problems tend to worsen during pregnancy, but, in one of the miracles of the human body, if your diabetes has been under control, your eye health usually returns to its pre-pregnancy status after delivery.
- Fetal electrocardiogram. Because there's a slightly higher risk of heart problems in the babies of diabetics, you'll probably get a special ultrasound of the fetal heart at about 22 weeks to make sure everything's going well.
- Tests of baby's well-being. There are a few tests you can expect, all with your and your baby's health in mind. For instance, the condition of your baby and the placenta will likely be evaluated throughout your third trimester with stress or nonstress tests and biophysical profiles. You'll also have regular ultrasounds to gauge baby's size and ensure she is growing at the right rate (and as you near delivery, that your little bundle isn't getting too big for a vaginal delivery). You may also be asked to count your baby's kicks three times a day after the 28th week to monitor fetal movements.
Last but not least, health providers know diabetics are at somewhat higher risk for preeclampsia, so your doctor will watch you closely for early signs of the condition. This means your practitioner will continue to check for elevated blood pressure and discuss any concerns or guidance about keeping it regulated, such as by exercising regularly and eliminating any stress (where possible).
Elective early delivery with diabetes during pregnancy
Women who develop gestational diabetes, as well as women with preexisting mild diabetes that is well controlled, can usually carry to their due date safely — though their babies are a bit more likely to be born prematurely. However, when Mom's normal blood sugar levels haven't been well maintained, the placenta deteriorates early on, or other problems develop late in pregnancy, your little bundle may be delivered a week or two before term.
The various tests mentioned above help a physician decide when to induce labor or perform a C-section — late enough so the fetal lungs are sufficiently mature to function outside the womb, but not so late that the baby's safety is compromised.
If your baby is delivered early, don't worry if she's placed in a neonatal intensive care unit (NICU) immediately after delivery. This is a routine procedure for babies born before 37 weeks.
Your baby will be observed for respiratory problems (which are unlikely if the lungs were tested and found to be mature enough for delivery) and for hypoglycemia (which, though more common in babies of women with diabetes, is easily treated). You should be able to get your baby back soon so you can start nursing, if that's your plan.
Feeding and caring for your baby after delivery
If you're planning to breastfeed, baby should nurse as soon as possible after birth, ideally within 30 minutes, and then every two to three hours to prevent hypoglycemia, or low blood sugar.
Be sure to talk with your doctor and get the hospital staff on board regarding feeding. The staff shouldn't test your baby's blood glucose levels until just before the second feed. This prevents any premature and incorrect diagnosis of hypoglycemia.
Check, too, that your baby isn't given formula or glucose water. Lastly, make it known that you'd like her brought to you regularly and early for continued feedings.
Complications of diabetes during pregnancy
Since diabetes affects almost every system in the body — brain, heart, skin, nerves, eyes and kidneys — failing to manage your glucose levels could put you at increased risk of a number of complications, from high blood pressure and preeclampsia to vision problems and even heart disease.
Babies of moms with unmanaged type 2 diabetes during pregnancy are also at increased risk of complications. If type 2 diabetes is not controlled properly during the first trimester, excessive sugar can affect the rapidly-developing fetal nervous system and comes with an increased risk of miscarriage.
In the second trimester, high fetal glucose levels can lead to macrosomia, a condition where a baby receives too many nutrients in the womb and is born larger than average.
Uncontrolled high blood sugar during pregnancy has also been linked to a number of other serious complications for babies, including heart problems, cleft palate, kidney and gastrointestinal tract disorders, brain damage, jaundice, hypocalcaemia (low calcium) and polycythemia (increase in red blood cells).
Babies of women with diabetes are also at higher risk for obesity and type 2 diabetes later in life.
While diabetes does put you and your baby at increased risk of complications during pregnancy, these risks are greatly diminished when the diabetes is managed effectively.
By taking control of your condition — closely monitoring your blood sugar, eating healthy, getting regular exercise and gaining the amount of weight that's right for you — you'll make a huge difference in the outcome of your pregnancy and the health of you and your baby, now and for many years to come.








































 Trending On What to Expect
Trending On What to Expect





